Breathing Pattern Disorders
IF YOU FEEL SHORT OF BREATH OR HAVE DIFFICULTY BREATHING, SPEAK TO A HEALTHCARE PROFESSIONAL
Breathing pattern disorders are abnormal respiratory patterns, often related to over-breathing and breathing more than what the body needs. They can range from simply using the wrong muscles, breathing only from the upper chest, mouth breathing, fast respiratory rate, large tidal volumes, and hyperventilation syndrome at the extreme end of the scale. You can find more detail on what breathing pattern disorders are from University Hospital Southampton NHS Foundation Trust, Physiotherapy for Breathing Pattern Disorders, Bradcliff and this research article titled “Getting to Grips with Dysfunctional Breathing”
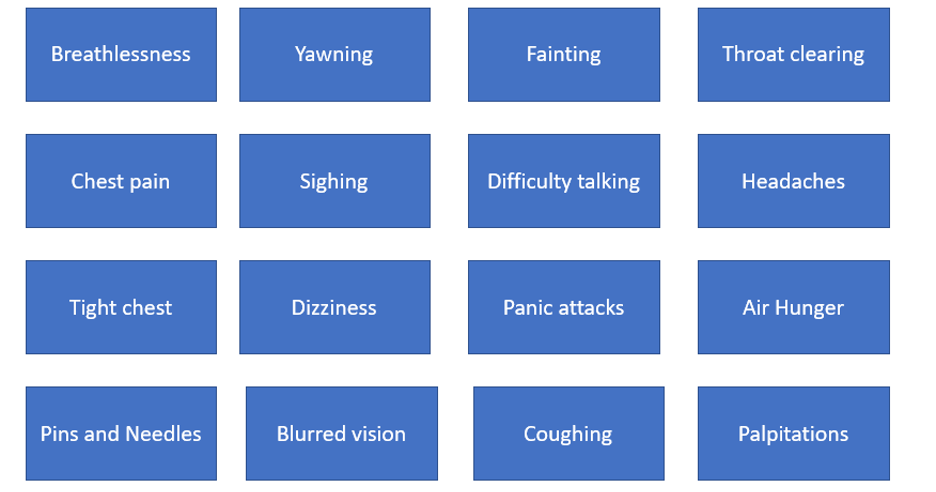
Over breathing can be a normal reaction to a range of stimuli and in the case of prolonged stressors or repeated triggers, this pattern can become a new normal. Stimuli or triggers can include illness, pain, stress, loss, anxiety, and worries in life. Over time, disordered breathing can cause a large variety of symptoms (image below).
Breathing pattern disorder is a complex syndrome that is difficult to define, but is described as a debilitating symptom, with a negative impact on quality of life, psychological wellbeing and functional status. It is a complex physiological problem derived from many potential causes. Physiotherapists play a key role in management of breathing pattern disorders.
How is Breathing Pattern Disorder Diagnosed?
People with breathing pattern disorder can present with a range of symptoms and investigations are important to rule out cardiac or other causes requiring urgent medical review so that the right treatment can be provided. Due to a range in presentations a diagnosis of breathing pattern disorder is not that of a disease confirmed by medical investigations. Respiratory Physiotherapists will listen carefully to peoples’ stories, assess symptoms and observe breathing. Some measurement tools (outcome measures) that may be used include the Nijmegen questionnaire. Questionnaires can be reviewed before and after treatment to determine effectiveness. In addition, the amount of carbon dioxide (C02) exhaled, can be measured using capnography. The faster a person breaths, the more C02 is exhaled, which in turn lowers whole body pH levels causing some of the symptoms experienced. Recently, the Breathing Pattern Assessment Tool (BPAT), a semi-quantitative screening tool used in the severe asthma population, has been included as an assessment tool in assessment of people with Long COVID.
What Causes Breathing Pattern Disorder?
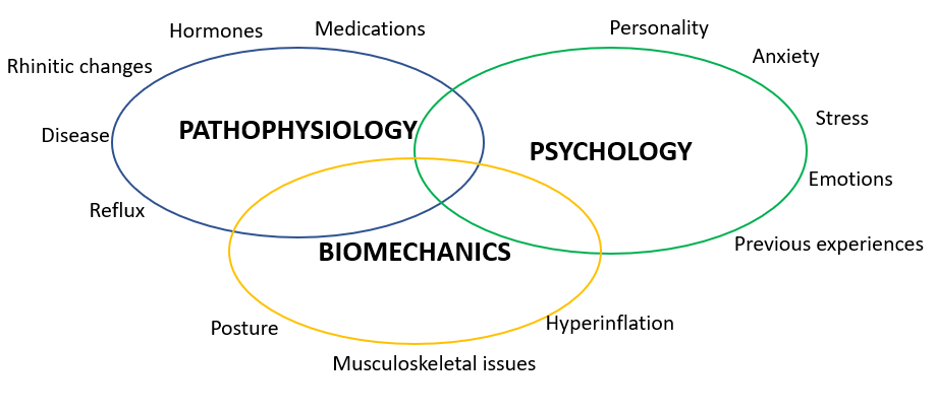
There are many triggers for a breathing pattern disorder and COVID-19 seems to be one of them where breathing patterns change during acute illness without returning to normal and this new way of breathing becomes the “new normal”. There is a complex interaction between pathophysiological, psychological and biomechanical causes and the triggers and issues will be different for everyone.
There is limited data on how common breathing pattern disorders are among people with Long COVID, the causes, long-term implications, or best practice for managing people with breathing difficulties. However, many people are still symptomatic many months after infection with COVID-19. A holistic package of care is recommended to address ongoing breathlessness.
What are the Treatments and Strategies for Managing Breathing Pattern Disorder?
The first step is education. Understanding how breathing works, what normal patterns are and how breathing patterns contribute to symptoms is essential. Armed with that knowledge, the next step is awareness. It is important that people can tune in to their own body and become aware of their own breathing patterns at different times, but specifically when symptomatic. Being aware of a dysfunctional breathing pattern helps in trying to establish a new functional pattern.
With knowledge and awareness, breathing retraining can begin. Typically, the focus is on three things with breathing: NOSE, LOW and SLOW. These self help videos support the advice below.
The NOSE is an essential part of the respiratory system and the aim is to manage nose breathing at all times (inhale and exhale) at rest. The nose functions to condition the air for the lungs - that is, it will warm the air, humidify it and filter (clean) it. It also sets up a natural resistance that helps the diaphragm to contract. Physiotherapy for Breathing Pattern Disorder provides a guide to breathing through your nose.
Which takes us to the next step: LOW. This means engaging in “belly” breathing. The diaphragm is our main breathing muscle and it contracts on inhalation, moving down into the abdominal cavity. To maintain abdominal pressures, the stomach muscles lengthen, causing the belly to expand outward - “belly breathing.” It is important that belly breathing is not confused with “big breathing”. Resting breathing volumes (tidal volume - the amount of air moved with each breath) is really quite small - only about 10% of full lung volume. It doesn’t take much effort or movement to perform resting belly breathing. Ideally, there is not a lot of chest expansion, or upward movement of the chest or shoulders.
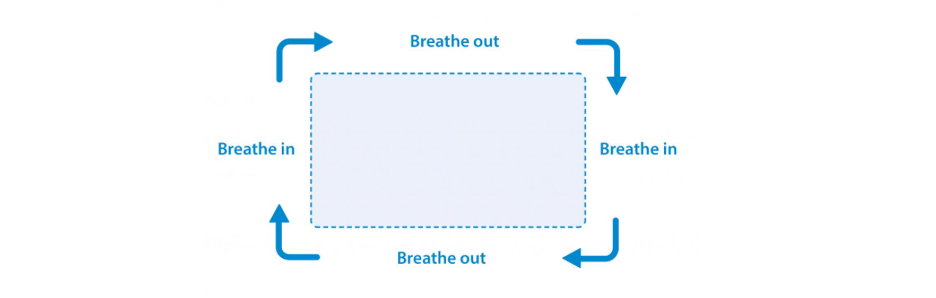
The last thing to work on is SLOW breathing. The aim is to establish a breathing rate of 8-12 breaths per minute at rest. A slower breathing rate, typically, allows for a slower heart rate, which may be important for people with Long COVID experiencing high heart rates (including dysautonomia). To slow breathing down, the breath out (exhale) needs to be a little longer than the breath in (inhale). This doesn’t mean squeezing air out of the lungs using a forced exhale, rather the key is to encourage the body’s natural breathing rhythm. At rest, inhale is active - relying on the breathing muscles (diaphragm and intercostals) to draw air in. The result is that the air moves quickly into the lungs. The exhale at rest is passive, relying on the elastic recoil of the lungs and diaphragm. This results in a slower flow of air out, thus, taking longer to complete an exhale. Slower breathing (generally achieved by lengthening the exhale) can help lower heart rate, improve parasympathetic nervous system activity and facilitate relaxation. The Association of Chartered Physiotherapists in Respiratory Care provide advice on how to cope with feeling short of breath.
The British Lung Association highlights this longer exhale breathing, by encouraging people to imagine breathing around a rectangle. Once the relaxed tummy breathing technique is mastered, imagine or look at a rectangle. Follow the sides of a rectangle such as a book, door, TV or a picture on the wall with your eyes as you use relaxed tummy breathing. Gradually slow the speed at which your eyes move around the edge of the rectangle to slow your breathing.
STASIS provides a free breathwork programme for people living with Long COVID.
Physiotherapy for Breathing Pattern Disorders provides a free guide to help you recover from COVID-19.
World Physiotherapy provided a range of useful resources for #WorldPTDay 20201 available in nearly 60 different languages in their toolkit, including information sheets on Breathing Exercises.
Relaxation, nutrition, rest and sleep are all important aspects of managing breathing pattern disorders, with more information available from University Hospital Southampton NHS Foundation. Some ideas to reduce activity of the upper chest muscles, available on Physiopedia, include:
Sit in an armchair. Rest arms on armrests. During breath in (inhalation), lightly press down on arms (minimal force to be applied).
Interlock hands with palms facing upwards. On the breath in (inhalation), push finger pads together
Interlock the fingers behind the head in supine (ie beach pose)
Sit forward on a chair and let arms drop so palms are facing forward. On the breath in (inhalation), turn the palms out
Stand with hands in front of the body. Grasp wrist with other hand and pull very lightly on the wrist
Provincial Health Services Authority Canada provide symptom management facts sheets on “Breathlessness” in English, Punjabi, Tagalog, and Traditional Chinese.
To read a story (blog) by a Physiotherapist living with Long COVID experiencing breathing pattern disorder click here.
The information on this page was written by Physiotherapists living with Long COVID and respiratory Physiotherapists specialising in breathing pattern disorders.
Date Last Revised: 9th September 2021