Long COVID
After having Coronavirus Disease (COVID-19), many people will start to feel better in a few weeks. Unfortunately, some people take a lot longer to get better. Having ongoing or new symptoms after COVID-19 infection is now widely recognised. These symptoms can change, come and go, or fluctuate over time. To describe these symptoms, people and healthcare professionals may use different terms. Long COVID is one of those terms, which was made by patients. The World Health Organization European Region Office have published a factsheet (2022) on Long COVID. The National Institute of Health and Care Excellence (NICE), Scottish Intercollegiate Guidelines Network (SIGN) and Royal college of General Practitioners published a booklet (2020) about Long COVID.
The World Health Organization Director General Dr Tedros Ghebreyesus, has stated the data is clear that Long COVID is devastating people’s lives and livelihoods, wreaking havoc on health systems and economies, therefore urging countries to launch immediate and sustained efforts to tackle this very serious crisis.
This episode is from the Long COVID Video Series. Please visit the website to access audio and written versions and translations.
Other terms that have been used to describe Long COVID include “Post-COVID Syndrome” (United Kingdom), “Post COVID-19 Conditions” (World Health Organization) or “Post-Acute Sequelae of COVID-19” (abbreviated to PASC) (United States). World Health Organization regional office for Europe and National Institute for Health Research (NIHR) have used the term Long COVID. “Post COVID-19 Conditions” is the term now used by the World Health Organization and United States Centers for Disease Control and Prevention (CDC). There are clear reasons why we need to keep using the patient-made term Long COVID.
This episode is from the Long COVID Video Series. Please visit the website to access audio and written versions and translations.
Long COVID has been coded in both ICD-10 CM (U0.9 + specific condition) and ICD-11 (RA02 + specific condition) for the purposes of recognition, data analysis, health service planning and delivery. The World Health Organization published their case definition of Long COVID in October 2021, developed through a Delphi consensus published in The Lancet December 2021. They defined Long COVID as:
“Post COVID-19 condition occurs in individuals with a history of probable or confirmed SARSCoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis. Common symptoms include fatigue, shortness of breath, cognitive dysfunction but also others* and generally have an impact on everyday functioning. Symptoms may be new onset following initial recovery from an acute COVID-19 episode or persist from the initial illness. Symptoms may also fluctuate or relapse over time.”
Long COVID is a condition where the underlying mechanisms or causes are not yet well understood. However post-viral conditions are not new, such as Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME/CFS). We know that some people continue to experience symptoms and ill health after first having symptoms of COVID-19. The mechanisms by which the infection leads to Long COVID are not yet fully understood. The underlying mechanisms are still largely unknown, but hypotheses include inflammatory or autoimmune processes, organ damage and scarring, hypercoagulability, persistent clotting, endothelial damage, or persistent viral protein in the body. In the scientific journal NATURE (Feb 2022), a publication outlines the existing knowledge of organ-specific sequelae of post-COVID-19 syndromes and examines the underlying pathophysiological mechanisms available so far, elaborating on persistent inflammation, induced autoimmunity and putative viral reservoirs.
Long COVID can affect people hospitalised with COVID-19 and people who were not admitted to a hospital. There is growing evidence that people who experience both mild or severe COVID-19 can experience Long COVID. We also now know that Long COVID is not just a short lived respiratory illness, and reinfections with SARS-CoV-2 increased the risk of Long COVID. Long COVID is a prolonged illness with multi-organ impairment, episodic disability, and serious implications for individuals and society including reduced participation in work or the labour market. Long COVID is associated with a greater likelihood of unemployment and lesser likelihood of being able to work full-time. Research helps us understand much more about Long COVID, however there is an urgent need to prevent Long COVID and to better understand the pathophysiology and underlaying causes of Long COVID.
It has been reported that people living with Long COVID can experience many different types of symptoms across different body systems. A list of common symptoms is available on the NHS website, CDC website, this booklet, and NIHR evidence reviews (first and second), patient-led research describes more than 200 symptoms, with 62 symptoms significantly associated with previous SARS-CoV-2 infection.
This episode is from the Long COVID Video Series. Please visit the website to access audio and written versions and translations.
It is difficult to know how common Long COVID is because estimations vary greatly, and self-reported symptoms may not reflect coding in electronic health records. It has been estimated that 144.7 million people globally were living with Long COVID in 2020 and 2021. In the United States, 1 in 5 people aged 18–64 years, and 1 in 4 aged ≥65 years, are estimated to have Long COVID after COVID-19 infection, with twice the risk for developing pulmonary embolism or respiratory conditions. A Scottish population cohort of 33,281 laboratory-confirmed SARS-CoV-2 infections, 6% had not recovered and 42% only partially, with previous symptomatic infection associated with poorer quality of life and impairment across all daily activities. In Canada about 1.4 million Canadian adults or 4.6% of the Canadian population aged 18 years and older, have symptoms at least 3 months after acute COVID-19 infection, with fatigue (72.1%), cough (39.3%), shortness of breath (38.5%) and brain fog (32.9%) the most reported Long COVID symptoms.
Some of the most representative Long COVID prevalence data comes from the Office for National Statistics (ONS), publishing reports in January 2021, April 2021, June 2021, July 2021, August 2021, September 2021, October 2021, November 2021, December 2021, January 2022, March 2022, May 2022, June 2022, August 2022, September 2022, October 2022, November 2022, December 2022, January 2023, February 2023 and March 2023. A technical report was published 16th September 2021 on Long COVID prevalence after infection, measured with different approaches. An accompanying blog by Daniel Ayoubkhani, explains why caution is required in interpreting results. Data specific to self-reported Long COVID after infection with Omicron variant is first reported in May 2022.
Data published in March 2023 estimates 1.9 million people living with Long COVID in the UK (2.9% of the population). This estimate varies compared to 2.0 million (3.0%) in February 2023, 2.1 million (3.3%) in January 2023, 2.2 million (3.4%) in December 2022, 2.1 million (3.3%) in November 2022, 2.3 million (3.5%) in October 2022, 2.0 million (3.1%) in September 2022, 1.8 million (2.8%) in August 2022, 2.0 million (3.1%) in June 2022, 1.8 million (2.8% ) in May 2022, 1.7 million (2.7%) in April 2022, 1.5 million (2.4%) in March 2022, 1.3 million (2.0%) in January 2022, and 1.2 million (1.9%) in November 2021. Of people with Long COVID in the March 2023 report, 83,000 (4%) first had COVID-19 less than 12 weeks previously, 1.7 million people (92%) first had COVID-19 at least 12 weeks previously, 1.3 million (69%) at least one year previously, and 762,000 (41%) at least two years previously. Of people with self-reported long COVID, 545,000 (29%) first had (or suspected they had) COVID-19 before Alpha became the main variant; this figure was 247,000 (13%) in the Alpha period, 327,000 (17%) in the Delta period and 698,000 (37%) in the Omicron period.
Disability was experienced by the majority of people living with Long COVID in the March 2023 report, whereby symptoms that adversely affect a person’s ability to perform day-to-day activities were reported by 1.5 million people (72% of those with self-reported long COVID), with 381,000 (20%) reporting that their ability to undertake their day-to-day activities had been “limited a lot”. Fatigue continued to be the most common self-reported symptom of long COVID (72%), followed by difficulty concentrating (51%), muscle ache/pain (49%) and shortness of breath (48%). As a proportion of the UK population, the prevalence of self-reported long COVID was greatest in people aged 35 to 69 years, females, people living in more deprived areas, those working in social care, those aged 16 years and over who were not working and not looking for work, and those with another activity-limiting health condition or disability. Around 1 in 20 people aged 16 years and over who were not in and not looking for paid work were experiencing self-reported Long COVID as of 2 July 2022.
Long COVID is legally classified as a disability in the United States under the Americans Disability Act (ADA), Section 504, and Section 155.
Source: Office for National Statistics - Coronavirus (COVID-19) Infection Survey (CIS)
Data identifies there was no statistical evidence of a difference in risk of Long COVID between first infections compatible with the Delta and Omicron BA.1 or BA.2 variants among triple-vaccinated adults.
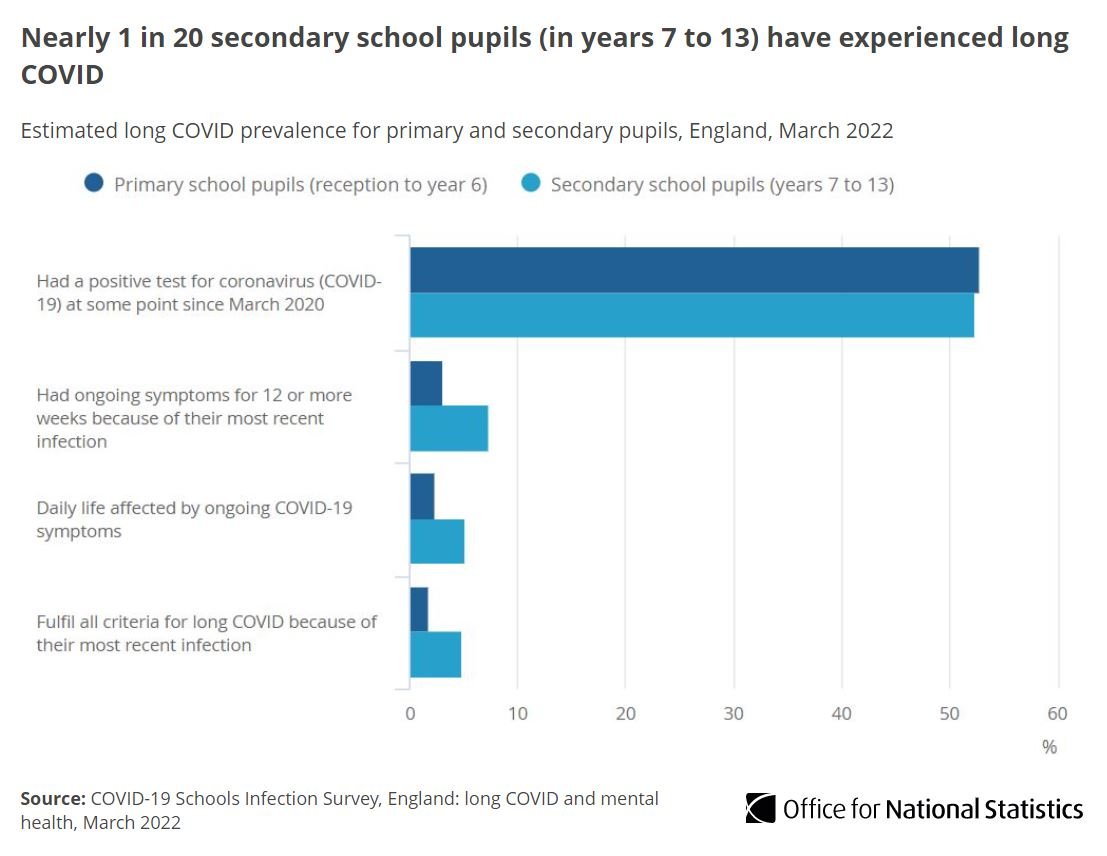
Long COVID also affects children and young people, with as many as 1 in 7 children living with Long COVID in the UK experiencing symptoms 15 weeks after infection with COVID-19. Long COVID is real and experienced by children and young people, with data demonstrating Long COVID symptoms are associated with SARS-COV-2 virus infection. The CDC reports children and adolescents are at risk of certain post COVID symptoms and conditions including acute pulmonary embolism, myocarditis and cardiomyopathy, venous thromboembolic event, acute and unspecified renal failure, and type 1 diabetes. Nearly 1 in 20 secondary school pupils have experienced Long COVID in England, as reported in the COVID-19 Schools Infection Survey. Data published by Office for National Statistics in the COVID-19 Schools Infection Survey (November - December 2021) estimates 1.0% or primary school-ged pupils and 2.7% of secondary school-aged pupils met criteria for Long COVID. Data was also published in July 2021. Compared to controls, children aged 0-14 years who had a SARS-CoV-2 infection had more prevalent long-lasting symptoms.
Long Covid Kids Support Pack
The Real Time Assessment of Community Transmissions (REACT-2) Long COVID sub-study estimated that among 508,707, 37.7% of 76,155 symptomatic people post COVID-19 experienced at least one symptom, while 14.8% experienced three or more symptoms, lasting 12 weeks or more. This meant over 2 million people in England were thought to have had Long COVID in June 2021.
Find out more from Long COVID Kids.
The National Institute of Health Research (NIHR) have provided two evidence reviews on living with Long COVID. Their first review was published in October 2021. Their second review published March 2021. In March 2021, the journal Nature Medicine published a comprehensive review of current literature on Long COVID including the pathophysiology, and in August 2021 published a systematic review and meta-analysis of the more than 50 long term effects of COVID-19. The Patient Led Research Collaborative published the most comprehensive patient-led research characterising Long COVID in an international cohort, describing over 200 different Long COVID symptoms. The UK Parliament published a rapid responce to Long COVID in December 2021, outlining the long-term health effects of COVID-19.
The ONS have published the social impacts of living with Long COVID, with Long COVID negatively affecting well-being, ability to exercise, and participation in work among people living with Long COVID in the UK.
The National Institute of Health and Care Excellence (NICE) published their first rapid guideline on managing Long COVID in December 2020, and updated in November 2021. They described Long COVID as the presence of signs and symptoms that develop during or following an infection consistent with COVID-19 which continue for 12-weeks or more and are not explained by an alternative diagnosis. This includes both ongoing symptomatic COVID-19 (from 4 to 12 weeks) and long term consequences of COVID-19 (12-weeks or more).
A core outcome set has been proposed from an international Delphi consensus study ‘PC-COS’, for research and clinical practice in Long COVID.
Long COVID has been characterised by different groups of people living with Long COVID as prolonged with multi-system involvement and significant disability, with an episodic, fluctuating, or relapsing nature.
This episode is from the Long COVID Video Series. Please visit the website to access audio and written versions and translations.
Physiotherapists living with Long COVID have described Long COVID as multi-dimensional, episodic and unpredictable in nature. The episodic nature of Long COVID is explored in this BMJ Global Health commentary. World Physiotherapy have published a briefing paper on safe rehabilitation approaches for people living with Long COVID. World Physiotherapy provided a range of useful resources for #WorldPTDay 20201 available in over 60 different languages in their toolkit, including information sheets on What is Long COVID and Long COVID and Rehabilitation. Exercise intolerance observed in Long COVID is not physical deconditioning and it is unacceptable to be simplistic when attempting to unravel mechanisms of exercise intolerance in people living with Long COVID.
Data is emerging on the potential risks factors of Long COVID, including female sex, belonging to an ethnic minority, socioeconomic deprivation, smoking, obesity and a wide range of comorbidities. The risk of developing Long COVID is also found to be increased along a gradient of decreasing age.
There are to date no known safe and effective treatments for people living with Long COVID. It has been reported that vaccines can change symptoms experienced by people living with Long COVID, as well as vaccines reducing the risk of people developing Long COVID. The UK Office for National Statistics (ONS) has reported how vaccines can reduce symptoms experienced by people living with Long COVID, with receiving 2 doses associated with a 9% decrease in the likelihood of reporting Long COVID symptoms that effect day-to-day activities. Recommendations have been published by Doctors living with Long COVID, for the recognition, diagnosis and management of Long COVID. Anitihistamines have been suggested as a potential pharmacological management.
People living with and effected by Long COVID have amassed vast experience about their own condition, and should be regarded as experts. An editorial in The Atlantic outlines current knowledge and areas for development about Long COVID, research and calls from community.
This episode is from the Long COVID Video Series. Please visit the website to access audio and written versions and translations.
Date Last Revised: 30th March 2023
You can access information about Long COVID in our QUICK ACCESS page, and in different languages on the links below.